Disposable Syringe Patented Tip Eliminates Dead Space in Vials
A new disposable syringe with an integrated (or stand alone blunt cannula) patented GlyFlo Technology tip can completely extract costly medications from rubber stopper vials and deliver them to patients effectively.
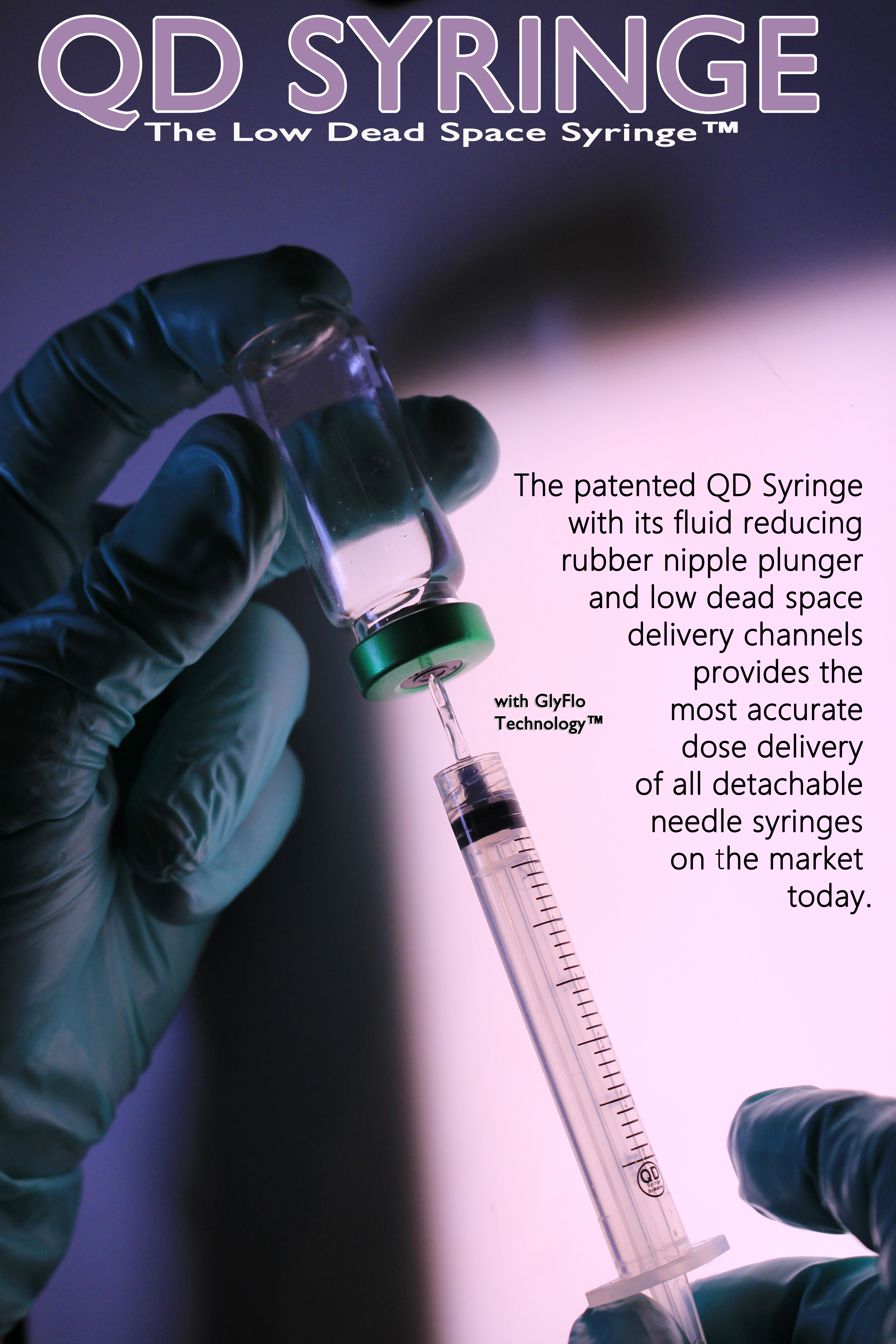
The QD Syringe Systems Quick Draw (QD) Syringe is a based on a solid acrylic dual-channel, draw-down tip which completely draws all medication out of a vial. An extended rubber nipple tip eliminates the dead space within the syringe, along with the proprietary GlyFlo Tip that reduces the dead space to only 18 microliters. Once medication is drawn into the QD Syringe, a custom hub with a sharp steel needle is placed over the draw tip, ensuring the sharpest needle possible when giving a patient an injection.
Because of the high dead space in current basic syringes, blood can linger on the tip and inside the hub, potentially encapsulating dangerous living pathogens for many weeks. However, the QD Syringe has a blunt tip with bilateral drying channels, which causes blood not to pool in the hub, reducing the spread of infectious diseases and protecting medical staff. In addition, the Quick Draw Syringe is made of a Bisphenol A (BPA)-free polypropylene body and a strong BPA-free acrylic tip, which increases patient safety.
“With so many changes in technology, we decided that there was a great need for not just a new disposable syringe but one that vastly improved the function, safety and efficiency of it. And with the rising costs of healthcare, there was also a need for a basic syringe that was cost-effective,” said Christopher Green, CEO and co-founder of QD Syringe Systems. “The QD Syringe simplifies the process of withdrawing medication from a rubber stopper vial and injecting it into a patient, or within seconds deliver medication into a patient’s luer access split septum.”
The basic Luer Lock syringe is dependent on two needles with hubs, one to draw the medication into its chamber and the second to deliver the medication to its intended patient. Current basic syringes waste up to 42 microliters in each separate draw needle, and up to 42 microliters are left in the vial. Often, up to another 84 microliters of residual medication are left in the syringe tip and hub after patient delivery, which that potentially up to 168 microliters of expensive medication is wasted.
________
The QD Syringe Systems has also created a QD Tip Blunt Plastic Cannula that can be lured on to ALL current basic 6% tapered syringes.
A New Syringe Designed for greater Dose Control ~ The patented design of the QD Syringe includes several innovative concepts that also help make it one of the most versatile syringe products available. The QD Syringe consists of a patented BPA Free cone tip with GlyFlo™ Technology designed as a ready to use draw down needle, eliminating time, needle dulling, hazardous waste and additional inventory ~ Unique bilateral fluid flow channels for easy draw and delivery of viscous liquids ~The QD Syringe is compatible with existing Luer Lock Hubs ~ The QD Syringe has a low dead space mating needle Hub available for up to 20 needle gauge sizes. The QD Syringe is a BPA Free Medical Syringe.
For More information contact: Christopher Green and Nicholas J. Sears, M.D., FACS at: Chris@qdss.us
Websites:
http://www.QDSyringe.com
http://www.QDSyringeSystems.com
_____